Geospatial Methods to Reduce Maternal Mortality in Paraguay
Spatial data is used to identify priority locations for care centers that can help Paraguay achieve progress on SDG 3.1, maternal mortality in addition to providing a wide range of benefits from improved access to care for rural populations.
Paraguay has set an ambitious goal to reduce its maternal mortality ratio to 40 per 100,000 by 2030, exceeding the SDG 3.1 target of 70 maternal deaths per 100,000 births. Progress has been made since 2005, as maternal deaths have decreased 17% from 159 to 132 per 100,000 in 2018. Yet these numbers are still more than three times higher than Paraguay’s target. What more can be done to ensure mothers are receiving the necessary care for safe pregnancies?
Since 2008 Paraguay has embarked on a vast expansion of its primary care network through centers known as Unidades de Salud de la Familia (USF), which offer an array of services, including prenatal care, blood sugar and pressure monitoring, and family planning. At a minimum, they are staffed with a doctor, nurse, obstetrician, and a team of community health workers, and are designed to serve between 3,500 and 5,000 people each in the country’s most excluded or high-poverty areas. The OECD’s 2018 Multi-Dimensional Analysis of Paraguay remarks that “increased access to higher quality health care during pregnancy and childbirth can prevent many of [Paraguay’s] maternal deaths… particularly for adolescent girls”. As such, Paraguay’s National Health Policy contains as a primary strategy the “strengthening of primary care centers, primarily through expanding and reinforcing the network of USF” (Gaete & Gauto) so as to achieve universal obstetric and neonatal care (ONC).
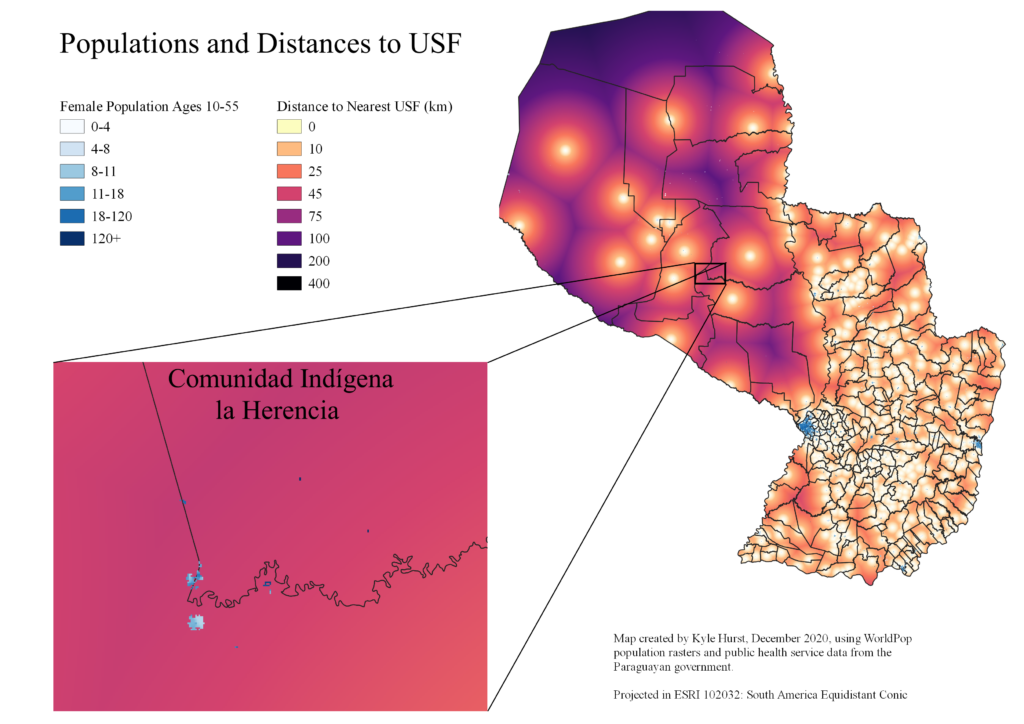
This focus on the expansion of primary care leads to the conclusion that there is a strong correlation between maternal mortality rates and primary care access. To examine this, I calculate each district’s average distance from a USF, then test the correlation between distance and mortality rates. I find a tentative negative relationship between the two, which is reflected in Figures 1 and 2. By my analysis, the average district, at a 0.05 per thousand maternal mortality rate, would see a 10% reduction in maternal mortality were it to reduce its total USF distance by 90%.
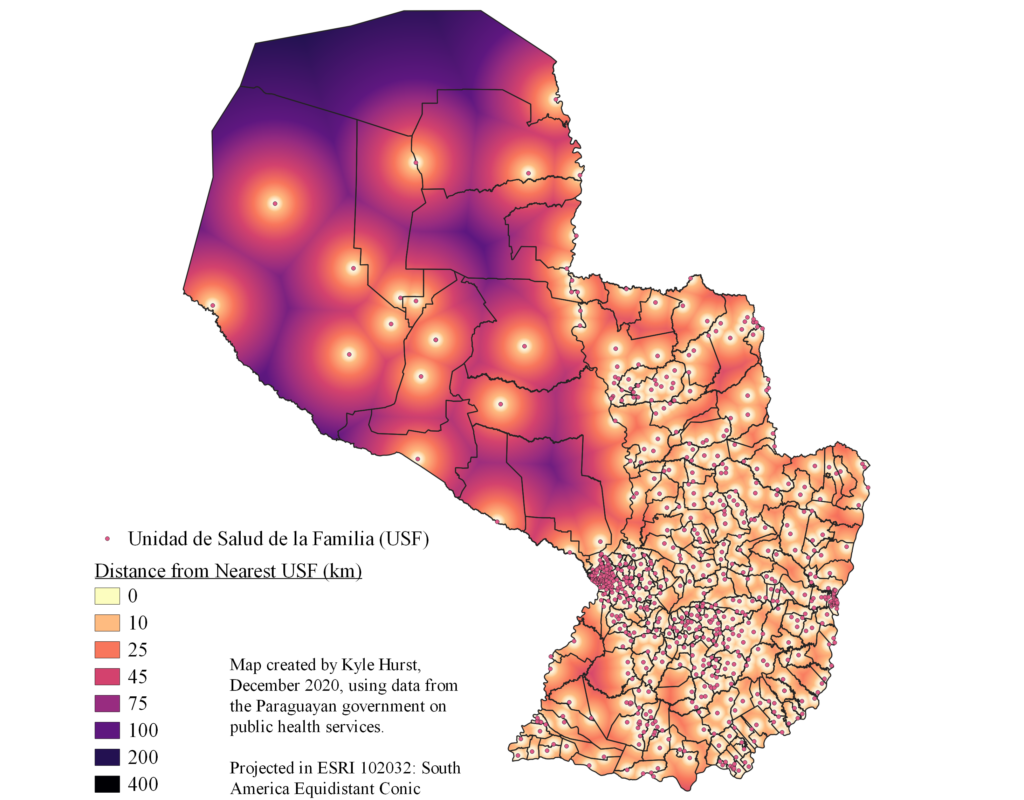
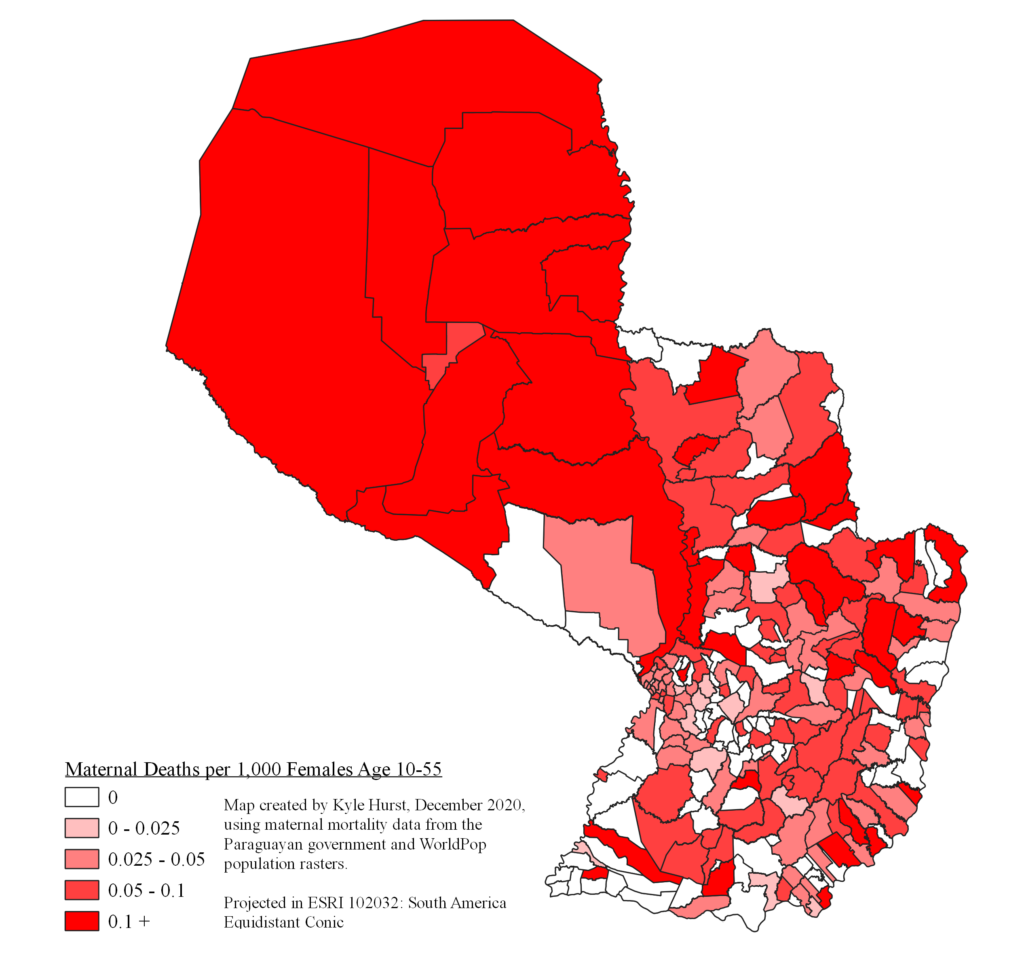
However, this relationship is by no means causal, as I lack both the granularity and the panel data necessary to make such an assertion. Factors such as per-capita GDP or clean water access may be omitted variables driving this correlation, and the targeting of USFs at high-poverty areas may bias my coefficients downward. Although the relationship between USF proximity and maternal mortality is tentative, there is still inherent merit in improving access to care. Paraguay’s goal of universal ONC, while related to the SDGs, is not designed entirely around the maternal mortality targets. Having understood this relationship, we can still use the distance calculations from Figure 1 to help identify underserved areas and potential candidates for a new USF.
Puerto Pinasco, located in the Chaco region of the country, has the country’s highest maternal mortality rate, and a total USF distance second only to Bahia Negra, one of Paraguay’s geographically largest districts. Yet Puerto Pinasco’s population is more than four times greater, suggesting more people live far from a USF here than in any other district. On the border of Puerto Pinasco and Villa Hayes lies Comunidad Indígena la Herencia (Figure 3). This area contains approximately 3,000 women between the ages of 10 and 55, suggesting its total population may exceed six or seven thousand. With this population, it easily meets the government requirement of 3,500 to 5,000 citizens per USF, yet it is about 50 kilometers from the nearest USF.
Belonging to an indigenous community once represented a severe obstacle to care access in Paraguay, but since 2008 these barriers are gradually being deconstructed. One of the principal triumphs of the USF project is that it has helped “bring basic health services to indigenous communities, who are now approaching the system with more confidence” (Zavattiero). In hopes of continuing this improvement, a new USF in La Herencia would be an effective improvement of the country’s primary care network. Its construction is also logistically feasible, given its location along one of the country’s principal highways. Although I hesitate to make any quantitative projection of this new USF’s impact on maternal health, previous literature and my findings in this study suggest it would produce positive results, and would certainly contribute to Paraguay’s goals of universal ONC.
My empirical analysis has offered tentative evidence of the efficacy of Paraguay’s primary care network of Unidades de Salud de la Familia. While neonatal care is but one of the services they offer, the USFs appear to correlate with lower maternal mortality rates in their nearby areas. My analysis also reveals ways in which the country’s health ministry might identify care gaps and better plan the expansion of its primary care network. Overall, my findings support the previous assertions that expanding and fortifying the USF network puts the country on a cost-effective path towards meeting its SDG 3.1 target. However, they do not by any means close the book on the matter, and there remain many aspects of Paraguay’s primary care system worthy of closer inspection.